The vast majority of our patients have had prior urethral stricture treatment that failed. In this case of bulbar urethral strictures, 90% have had 1 or more failed dilations and/or internal incisions (internal urethrotomy). These men are best managed with urethroplasty. The 2 most common approaches are urethral reconstruction with excision and primary anastomosis (EPA) also called anastomotic urethroplasty and a repair with the use of a patch of tissue from inside the cheek (for longer strictures, that likely became too long for EPA due to the prior treatment making the recurrent stricture longer). These urethoplasty operations at the Center for Reconstructive Urology have long term success rates of 95-99+%.
As more doctors without expertise and exclusive specialization in Male Reconstructive Urology are including urethroplasty as an one of their areas of expertise and having poor outcomes, we are seeing more men with recurrent strictures. These failed surgeries are performed at both major University teaching hospitals and by Urologists who in large group practices that want to offer all services. What is most alarming is that these men then have strictures that are considerably more complex than before the failed surgery. The following are several examples:
A 10-year-old boy was hit by a car and suffered a pelvic fracture urethral injury. He was taken to his local pediatric urologist, who performed a repair (posterior urethroplasty) that was complicated by an early failure. This is an operation we have performed for over 20 years with a 100% technical success rate. The urologist then performed another repair, which was also complicated by an early failure. He was then referred to the Center for Reconstructive Urology and a diagnostic evaluation revealed a total urethral obliteration.
Total Urethral Obliteration
The most likely cause of the repeated failure to repair the urethra was a lack of proximal exposure and incomplete removal of scarring around the damaged area. This is not uncommon wjen this surgery is performed by inexperienced surgeons, as their lack of expertise can lead to technical complications. We were able to successfully perform a complicated re-do re-do repair with complete scar excision, and the boy is now able to urinate normally.
When short bulbar urethral strictures are treated with anastomotic urethroplasty, this is a surgery where a small area of stricture is removed, and the 2 ends are sewn back together. If the is a recurrence, the recurrence should be at the area of the connection and involve a very short segment. However, we have seen recurrences as long as 11 cm after the repair of what should have been a very short stricture, since anastomotic urethroplasty is an option only for short strictures. We reviewed our data and found that after failed anastomotic urethroplasty, the average stricture length of patients coming to our Center for re-do surgery is over 6cm!
One patient was referred to our Center for a stricture that would have been highly amenable to a repair with anastomotic urethroplasty or the use of buccal mucosa. However, when he was re-directed by his insurance to a different major University teaching hospital in an adjacent county where he underwent a surgery that used scrotal skin as a patch to repair the urethra. A hair ball grew inside the urethra and the stricture recurred.
The insurance company then approved a re-do surgery at our Center, and that was a successful urethroplasty.
When the urethral strictures are long and/or there is a history of 1 or more failed prior surgeries, innovative urethral reconstruction surgeries are required. Wherever the urethra is narrow, tissue must be used to add to the narrow urethra to make it wider. Where there is a total obliteration, tissue must be added not only as a patch, but along the entire circumference of the urethra.
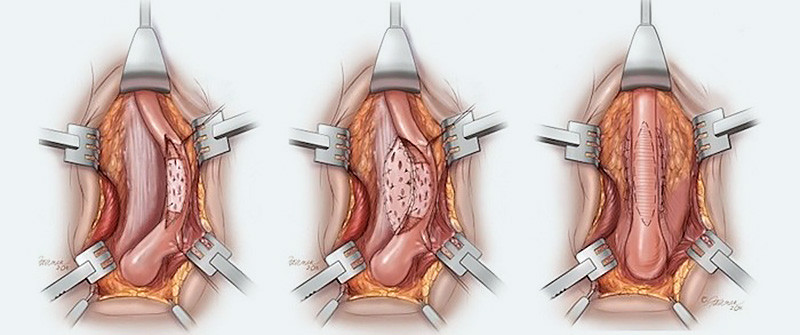
When there is a total obliteration of the penile urethra and there is excess penile skin available, we prefer to use a combination of penile skin (flap) and buccal mucosa graft to reconstruct the urethra. As shown in the graphic below, the penile skin is “de-gloved”, exposing the obliterated urethra. This allows us to then open the normal urethra at the base of the penis.
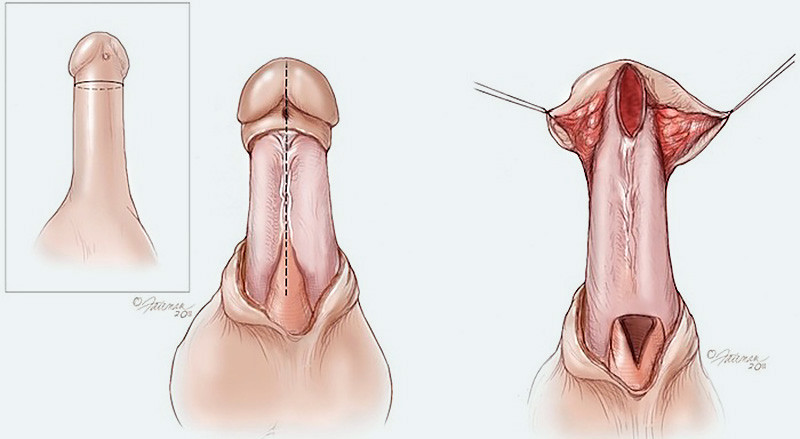
The buccal mucosa is then added along the undersurface of the penis to create a new strip of the urethra. The penile skin is then used to help complete the repair as the new urethra is tubularized. Our experience and success with this technique published in the Journal of Urology.
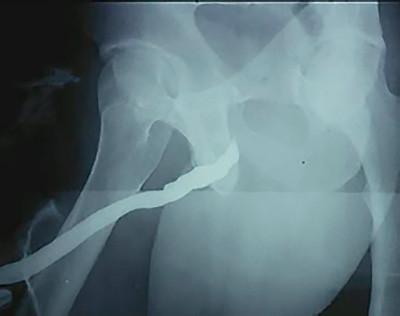
In 1999, a patient was referred to our institution after urethral stent placement and the subsequent removal of the stent led to complications that resulted in a 5 cm total obliteration of the bulbar urethra.
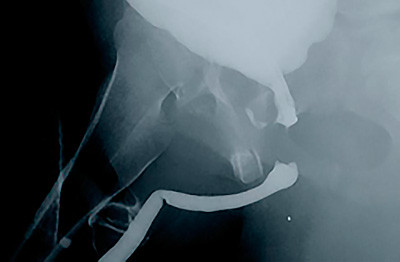
RUG of 5 cm Obliteration

Penile skin was not available, but even if it was, it has been reported that using tissues to reconstruct the entire circumference of the urethra generally leads to poor outcomes. One option to overcome this obstacle would have been using a two-stage repair process. However, through some ingenuity by Dr. Gelman, this patient’s urethra was instead reconstructed in one surgery using a new and innovative technique.
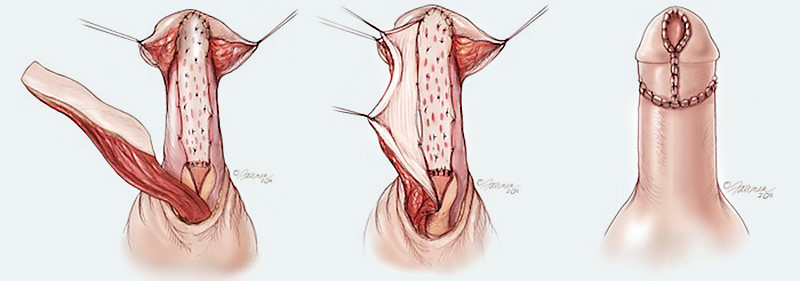
The first step was to make an incision under the scrotum. This incision, called a perineal incision, exposed the obliterated urethra. The next step was to rotate and cut open the structure that surrounds the urethra, called the corpus spongiosum. Then, we extended the incision all the way into the healthy normal urethra at both ends of the obliterative stricture, as shown below.
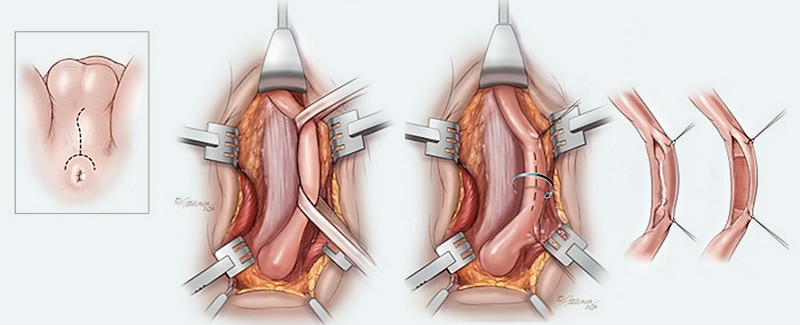
Buccal mucosa was then quilted to the corpus spongiosum to reconstruct a portion of the urethra (ventral portion), as shown below. Then a second graft was quilted to the undersurface of the penis, as previously described by Barbagli, to successfully patch and enlarge a narrow urethra. These two seperate grafts were then connected to form a tube.
A retrograde urethrogram taken three years following the successful surgery revealed no deterioration and a urethra with no signs of narrowing or closing. An 18-year follow-up evaluation revealed that this patient has not had a recurrent stricture and remains asymptomatic.
RUG After Repair
Inspired by the success of this new technique, Dr. Gelman has subsequently expanded the use of this technique and published his results in the journal Urology. This innovative new technique is now called the “double faced buccal graft” and this surgery has been adopted world wide as the preferred approach to strictures that include obliterated or nearly obliterated segments.
The approach to repair recurrent long strictures is individualized based on several different factors. Some of the factors that determine which approach will work best include the exact location and length of the stricture, whether there are multiple strictures, the availability of excess penile skin, as well as the integrity of the tissues surrounding the urethra.

