We often manage patients who have had repairs that have failed. Sometimes the urethral openings are still not placed correctly, and there is also not enough skin to use in the reconstruction of the urethral opening. This condition requires a complex approach that may include the use of skin grafts from other parts of the body. Although these repairs are more involved, and may require a staged approach, a successful outcome is often achieved.
The following case is an 8 year old boy who was born with hypospadias and underwent multiple failed surgeries. Ultimately he developed an inability to urinate and required a tube to be placed in his bladder to drain the urine so that the bladder could empty. Given the complexity of the case, he was then referred by his Pediatric Urologist at a major University to the Center for Reconstructive Urology for evaluation and treatment. On physical examination, he was found to have a urethral opening at the tip of the penis, and adequate penile skin.

Adequate Penile skin

Urethral opening at the tip of the penis
The urethral imaging, unfortunately, revealed that there was a stricture of the entire previously reconstructed urethra extending from the tip of the penis to the portion of the urethra next to the prostate under the scrotum.
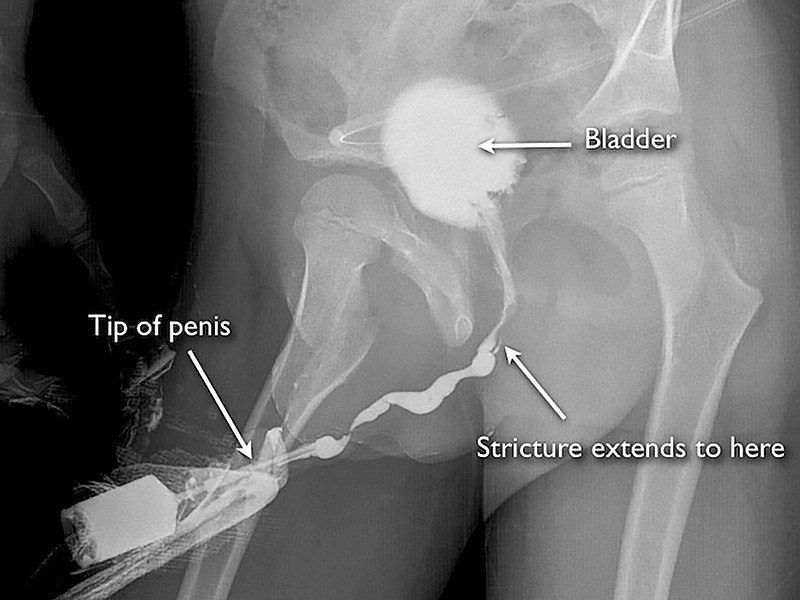
Retrograde urethrogram demonstrating severe pan-urethral stricture disease after prior hypospadias surgery
This problem is best managed with a staged urethral reconstruction using buccal mucosa grafts (tissue from inside of the cheek) and split-thickness skin grafts from the thigh.
When children undergo initial hypospadias surgery, penile skin may be used to reconstruct the urethra. If this surgery is complicated by breakdown of the repair and/or urethral stricture disease, some Pediatric Urologists will continue to use penile skin as it is readily available. However, one problem is that the penile skin blood supply is less reliabile after prior surgery and there is a risk of creating a penile skin deficiency with continued use of penile skin during multiple revision surgeries. When patients are left with severe deformity and/or stricture disease with penile skin deficiency, this is called a “hypospadias cripple”. However, that term is not currently favored to describe this unfortunate condition. The following is the example of an 18 year old who was born with hypospadias and underwent many repairs, including the use of a full thickness graft from the abdomen (not a standard technique). At the time of referral, he was found to have virtually no remaining penile skin along the undersurface of the penis and a bulky ball of scar at the base of the scrotum.

Undersurface of the penis

Severe penile skin deficiency
This patient did not have any significant penile length with erections and was sexually disabled. In these cases, the priority is to treat any urethral stricture disease and skin graft the penis (split thickness graft) so that sexual intercourse will be possible. At the conclusion of the surgery, there is no urethral obstruction and the penis will have adequate length for intercourse. However, the urethral opening will not be at the tip of the penis. Options at that point include staged urethral reconstruction or maintaining the urethral opening at the undersurface of the penis. In this case, we were able to subsequently reconstruct the urethra to bring the urethral opening along the distal shaft of the penis, but it was not practical to bring the opening to the tip of the penis. Staged urethral reconstruction after penile skin grafting is very problematic as the blood supply to the tissues is marginal. In these challenging cases, we can not always achieve a perfect cosmetic and functional result. However, we can generally create a situation where the patient can be sexually active and urinate without obstruction and have an improved cosmetic appearance of the penis.

