One of the greatest difficulties when it comes to comparing surgeons and specific surgical operations with regard to urethral stricture treatment results is that there is no agreed-upon definition of urethral stricture surgery success. This discrepancy means that the success rate reported by other urology centers may or may not actually be as impressive as it seems at first glance. At The Center for Reconstructive Urology, we have a rigorous process in order to declare a surgery a success. With this very strict interpretation of urethral stricture surgery success, our long-term success rate exceeds 95-99% for certain surgeries.
1. Success = Urine Flow Rate – Uroflow with success a flow rate of 12-15 ml/sec
In published literature, there are several definitions of success in the treatment of strictures. Some literature defines urethral stricture surgery success as a urine flow rate of at least 12-15 ml/second. However, the problem with this classification of success is that it is not a very high bar to clear. A normal flow rate is often greater than 35ml/sec.
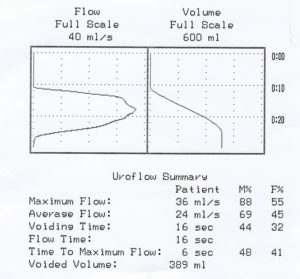
It is very possible for a patient to have significant narrowing of the urethra with a flow rate of only 12-15 ml/sec. For these reasons, a surgery can ultimately be unsuccessful in curing the patient of urethral stricture disease, but be deemed a success by the above definition.
2. Success = no further treatment or “absence of symptoms”
Another definition of success is if the patient did not have symptoms or did not require further surgery, even if that meant catheterizing himself to keep the urethra open. These papers often do not say how they define symptoms, even though there are research tested (called validated) questionnaires to objectively assess symptoms suggestive of urethral stricture disease recurrence. It is possible that those who did not “require” further treatment elected to not have further treatment for a recurrent stricture since the prior treatment did not work. If someone has to catheterize even once, that means the surgery did not cure the stricture. Moreover, “followup” is not always clearly defined. This can mean how long it was since the surgery (where the patient was never seen after surgery) or how long between the surgery and the last time the patient was contacted or seen. If one considers no news as being good news, then this favors a higher success rate than may be the case.
These definitions of success were often used in older published papers and literature reporting on the success of dilations and internal incisions called direct vision internal urethrotomy (DVIU). With these definitions of success, the success rate had been reported to be as high as 60+%. However, with a stricter definition of success, these procedures have been found to be curative in 0-8%
At the Center for Reconstructive Urology, since 1998, it has been our protocol to perform urethroscopy 4 months after surgery to assess the patency of the urethra and confirm that there is not a recurrence of the urethral stricture. For urethroscopy, we use a camera connected to a high-resolution monitor, allowing our patients to compare images of their stricture before surgery to the area of repair after surgery. We wait 4 months to allow the urethra to completely heal, allowing us to accurately confirm that no narrowing developed during the healing process. This follow-up is incredibly important. It is so important that when patients travel from out-of-state for care, we make sure prior to surgery that the patient is willing to return 4 months later for a follow-up. It is at this follow-up evaluation that we confirm technical urethral stricture surgery success. If the scope does not pass through the area repair easily with the urethra being wider than the scope, we call this a failure even if the urethra is way less narrow than before surgery and patient has no symptoms because our goal is to make the narrow urethra wide. It is always possible for a properly performed urethral surgery to fail within 4 months, but this should be a very rare occurrence, and not something that should happen in 10-15% of patients.
The 4-month follow-up evaluation is not the last time that surgery results should be evaluated. We stress the importance of an annual follow-up appointment each and every year following surgery. These appointments consist of a symptom assessment using a standardized validated questionnaire, a urinalysis, and a measurement of flow rate and residual urine volume (PVR). If the results of these tests lead us to believe that there is any concern of stricture recurrence, urethroscopy is advised to directly assess the caliber of the urethra. It is at these appointments and with the use of validated symptom questionnaires that we can continue to confirm long-term urethral stricture surgery success. We define long-term success as life-long wide patency of the urethra without recurrence which would then need treatment with dilation or a direct vision internal urethrotomy (DVIU) or catheterization or other treatment
The Center for Reconstructive Urology specializes in male urethral stricture surgery and we present our data at regional, national, and international meetings and we publish our results in the Journal of Urology, Urology, and other peer-reviewed journals.
Many of our patients are referred by their local Urologists, and many patients travel from out of town for care. We do not want to interfere with the relationship between a patient and their local doctors. Moreover, our out of town patients have travelled from 46 different states and 26 different countries for surgery, and it would be impractical for them to return annually indefinitely. Therefore, after the initial 4-month visit, we encourage patients to return to their referring or local Urologists for their annual follow-up and keep us informed of their progress. However, if the patient’s preference is to return to us each year, we are happy to provide this follow-up.
Unfortunately, as the years go on and patients show no signs of any stricture symptoms, many men stop making annual appointments. Patients also move and do not provide us with their new contact information. When this happens, patients become “lost to follow-up”. This is a prevalent problem for all Academic physicians who present and publish outcome data.
A publication may state that when XX number of patients had YY surgery, the urethral stricture surgery success rate was 90% with an average follow-up of 5 years. This could mean that with this followup, 90% of the patients have wide open urethras, or it could simply reflect how long ago on average the surgery was performed. The success rate can also be skewed by the possibility that some of the patients developed a recurrence and pursued further care elsewhere. One needs to look closely to see how success was defined and how many of the patients actually were followed up.
We are not immune to this problem, and we make a major effort to maintain contact with our patients. We strive for our outcome data to truly and accurately reflect our results. At the Center for Reconstructive Urology, we maintain a detailed database that has been prospectively maintained since 1998. This allows us to assess our results for any given procedure at any given time. We constantly update the database with any and all information, making a significant effort to maintain contact with our patients so that the data remains up to date. What makes this possible is the generous support of donors who contribute to our research efforts, and we have a full-time research coordinator who maintains our database. Our research is approved by the Institutional Review Board (IRB) of the University of California, Irvine.
Bulbar Strictures – Anastomotic Urethroplasty
For bulbar urethral strictures (commonly caused by straddle injuries), we recently reported an early success rate of 100% when anastomotic urethroplasty was performed (cut out the stricture when short then reconnect the healthy ends. This was always assessed by a look with a scope 4 months after surgery. The long-term success was 99.3% and for patients to be included, they had to complete validated questionnaires. This is the highest reported success rate and with the strictest definition of success.
Pelvic Fracture Urethral Injuries – Anastomotic Urethroplasty
For pelvic fracture urethral injuries, tears of the urethra that can happen when the urethra is severed from motor vehicle accidents or pelvic crush injuries, our early success rate has been 100% and long-term success has been 98%.
Dorsal Buccal Graft Onlay Urethral Stricture Repair
When bulbar strictures are too long to be treated with anastomotic urethroplasty, we add tissue of the narrow portion of the urethra to make it wider, and this is called dorsal onlay buccal grafting, a surgery made popular by Italian Urologist Guido Barbagli. With this technique, our early success was 97.5% and late success was 95%. It should be kept in mind that for some of our “failures”, the urethra may have been just slightly smaller than the size of the scope, but wide enough that the patient was without symptoms (in comparison to before surgery) and not needing any further treatment. Some would consider these patients to be a success, and we consider it a very beneficial thing when someone comes to our Center with a major problem, and then never has symptoms after a surgery. However, we maintain a very strict standard when reporting success rate.
Dorsal-Ventral Buccal Graft
Dr. Gelman has pioneered and published several new innovative techniques to treat complex urethral strictures. One such new surgical urethroplasty technique is now being called the “double faced buccal graft repair”. This was developed to provide a better way to repair long areas of urethral obliteration with a high success rate of 94%
More recently, we have used this operation that was once reserved for some of the most complex cases to treat men with longer strictures of the bulbar urethra where there is a particularly narrow segment with excellent results. Dr. Gelman’s double buccal graft urethroplasty technique is now becoming popular worldwide
Staged Repairs of Urethral Strictures
Among the more complex surgery cases are those that involve very long segments of the urethra including the urethra within the penis, and these often require a 2-stage repair where graft tissue is added to the urethra in the first operation, and then made into a tube 4 months later during the 2nd stage. This year, we presented our early and long-term success rates comparing the use of skin grafts and buccal grafts (tissue from inside the cheek)
Our early success rates were 100% success for both groups. However, we found that there were no late recurrences with the use of the buccal grafts and a fairly high recurrence rate years after the technically successful surgery when skin grafts were used. This is a reflection of the poor durability of skin grafts. As a result, we now favor buccal grafts.
When the success rate may not be 95-100%
When Dr. Gelman established the Center for Reconstructive Urology at UC, Irvine in 1998, he was 1 of only 3 Urologists in the western half of the United States with expertise in male urethral-genital reconstructive surgery. Recently, male Reconstructive Urology has become very popular and considerably more Urologists are performing urethoplasty surgery in the past 5 years than we have seen in the 10-15 years before that. As a result, we are seeing an increasing number of patients who come to us after failed urethroplasty. We can still offer these men re-do surgery with a very high success rate, but since these are considerably more complex problems, the success rate is not as high as for initial surgery. Our early technical success rate of 100% in treating men with anastomotic urethroplasty for bulbar strictures was for initial open surgery (although the vast majority had prior failed dilations and internal stricture incisions).
When the urethroplasty success rate will be lower
Patient Mr. T.T. was referred to our Center by his local Urologist. He was contacted by Dr. Gelman, and we scheduled a consultation and evaluation to determine the best treatment method. At the last minute, he cancelled and elected to seek care closer to his home. We followed up with the patient months later to confirm that he had received proper care.
He indicated that he had opted for treatment with a doctor at a major University Medical Center who was also a Reconstructive Urologist and this offered him some insurance cost savings and convenience. However, that Urologist’s practice was not exclusively devoted to Male Reconstructive Urology. He underwent urethral reconstruction for a short bulbar stricture that was 1-2 cm long with excision and primary anastomosis (also called anastomotic urethroplasty). The short stricture was removed and the ends are re-connected an operation that has been performed with a 100% technical early success rate over the past 20+ years at our Center.
After the surgery, the patient reported that he was given the impression that the surgery was considered a urethral stricture surgery success. However, he also stated he was required to return to the urologist for periodic catheter insertions, and that the catheter insertions were associated with significant bleeding. After informing the patient that he was not describing what should be considered a success, he elected to come to our Center for a diagnostic evaluation. A retrograde urethogram (RUG) was performed that revealed a 9 cm recurrent narrow caliber stricture.

By our definition, this patient did not have urethral stricture surgery success. He had an early failure of his surgery, resulting in a recurrent stricture that was significantly more complex than when he was originally referred to our institution prior to the surgery. The re-do surgery he required was a very extensive repair that included extensive tissue transfer and the use of more than 1 graft. This was the 1 patient in Dr. Gelman’s series of double-faced buccal grafts that had a recurrence.
With urethroplasty surgery, the highest success rate is during the first surgery.
